Resuscitation of pregnant women
The prevalence of cardiovascular arrest has risen in recent years due to the increase in anamnestic maternal risk constellations and the increase in pregnancy complications. Currently, the prevalence is 1/12,000 pregnant women.
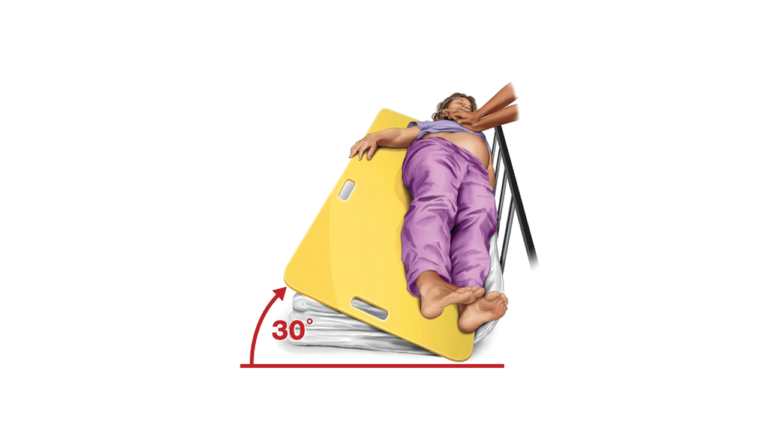
Cardiac massage in pregnant women - tips for optimising (aorto-) caval compression syndrome from the 20th week of gestation onwards
Venous return and fetal circulation can be negatively affected by aorto-caval compression syndrome from the 20th week of gestation in the supine position. Therefore, pregnant women are normally positioned in a 15-30 degree left lateral position (Figure 2). In the left lateral position, however, CPR is problematic and chest compressions are significantly more difficult.
Therefore, it is currently recommended to displace the gravid uterus to the left with both hands by an additional assistant during resuscitation (Figure 1). This ensures maternal and fetal circulation as best as possible during resuscitation.
What happens to the unborn child?
If the situation arises that only an emergency caesarean section can save the life of the mother and/or the child, the following procedure is recommended:
Up to the 24th week of pregnancy (SSW)
Here, an emergency caesarean section is not recommended because the pregnancy is very unlikely to have any influence on the mother's survival. Moreover, up to the 23rd week of gestation, it can be assumed that the child has only minimal chances of survival.
From the 24th week of pregnancy
An emergency caesarean section may be considered here, as the pregnancy may have a negative impact on the mother's survival. The primary goal here is to save the mother. This is because the chances of survival of the child are generally considered to be very low under resuscitation.
What exactly is improved for the mother by the emergency caesarean section?
- the mother's oxygen consumption is reduced
- venous return is improved (aorto-caval compression syndrome)
- the mother's lung mechanics are optimised as the intrathoracic pressure decreases.
In general:
The life of the mother always takes precedence over the life of the unborn child.
Conclusion:
Only 2 things can ensure the survival of a pregnant woman
Only with high-quality chest compressions and the early use of an AED (automated external defibrillator) can a pregnant woman most likely be saved.
High-quality cardiac massage and the immediate use of a defibrillator are among the Grade 1 recommendations of emergency medicine and are therefore crucial for the victim's chance of survival.
To optimise the potential for aorto-caval compression syndrome (from 20 weeks gestation)I, a second assistant should use both hands to displace the gravid uterus to the left during CPR.
Furthermore, every resuscitation of a pregnant woman is an exceptional psychological situation for everyone involved, which certainly makes your work even more difficult.
Defibrillation in pregnant women
- The same impedance in pregnant as in non-pregnant women (biphasic defibrillation energy: 120-360 joules, escalating).
- Fetal exposure to electrical energy is minimal = no danger to the child (current flow through the uterus/amniotic fluid, decisive factors are current strength and contact duration).
- The changed anatomy during pregnancy makes the use of pads more difficult → Use adhesive electrodes
- Arcing to external or internal fetal monitoring units is unlikely (single case reports), therefore they do not need to be removed during current application. This avoids a delay in defibrillation.